Medical Billing Audit Template
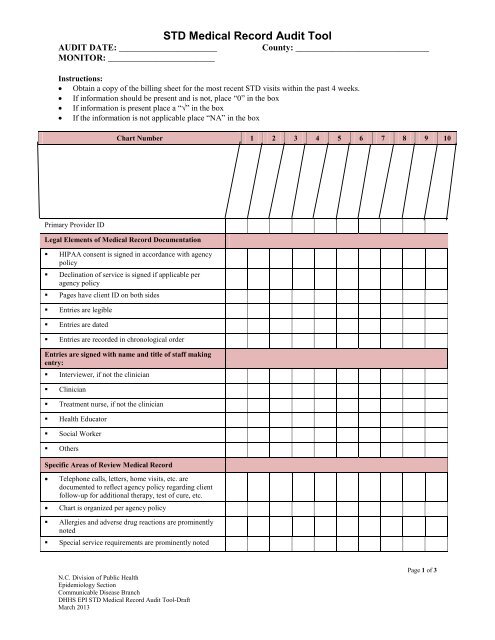
Professional review audit checklist 1 is there an appropriate tool to correspond the services rendered to the professional billing entity.
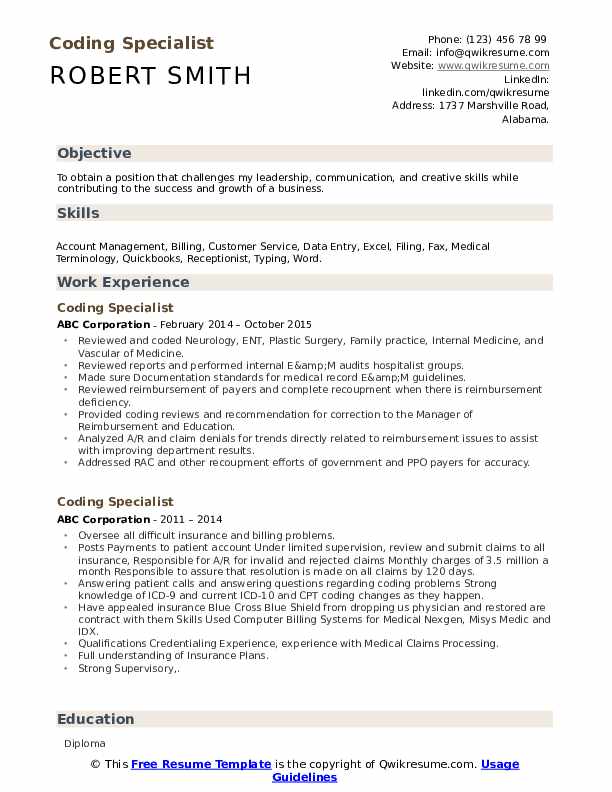
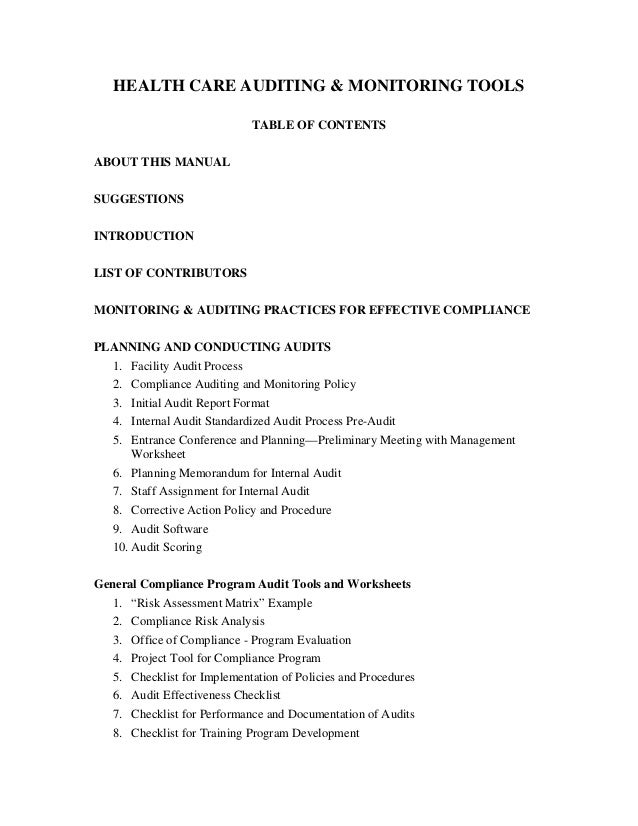
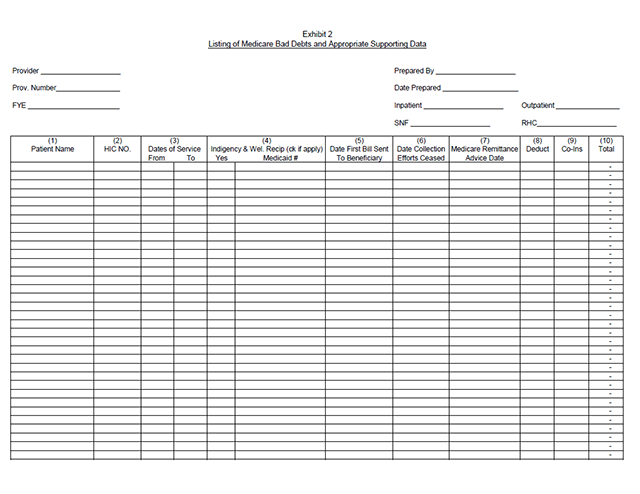
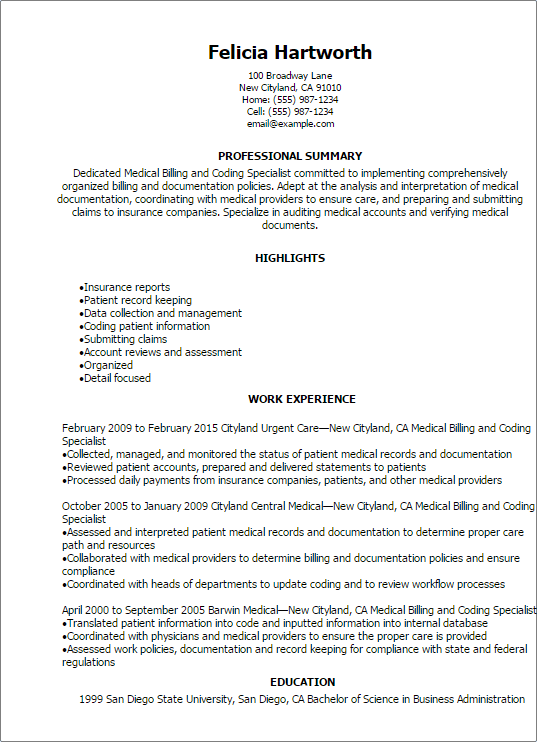
Medical billing audit template. This can improve the quality of care your practice provides as well as potentially generating revenue improvements. The practice has designated a compliance officer to oversee and monitor compliance with fraud and abuse laws in addition to other regulations. Billing audits are one approach to fix this problem. The scope of a medical billing audit is limited and is intended to verify charges on the detailed claim are accurate represent services rendered to the patient and are ordered by a physician.
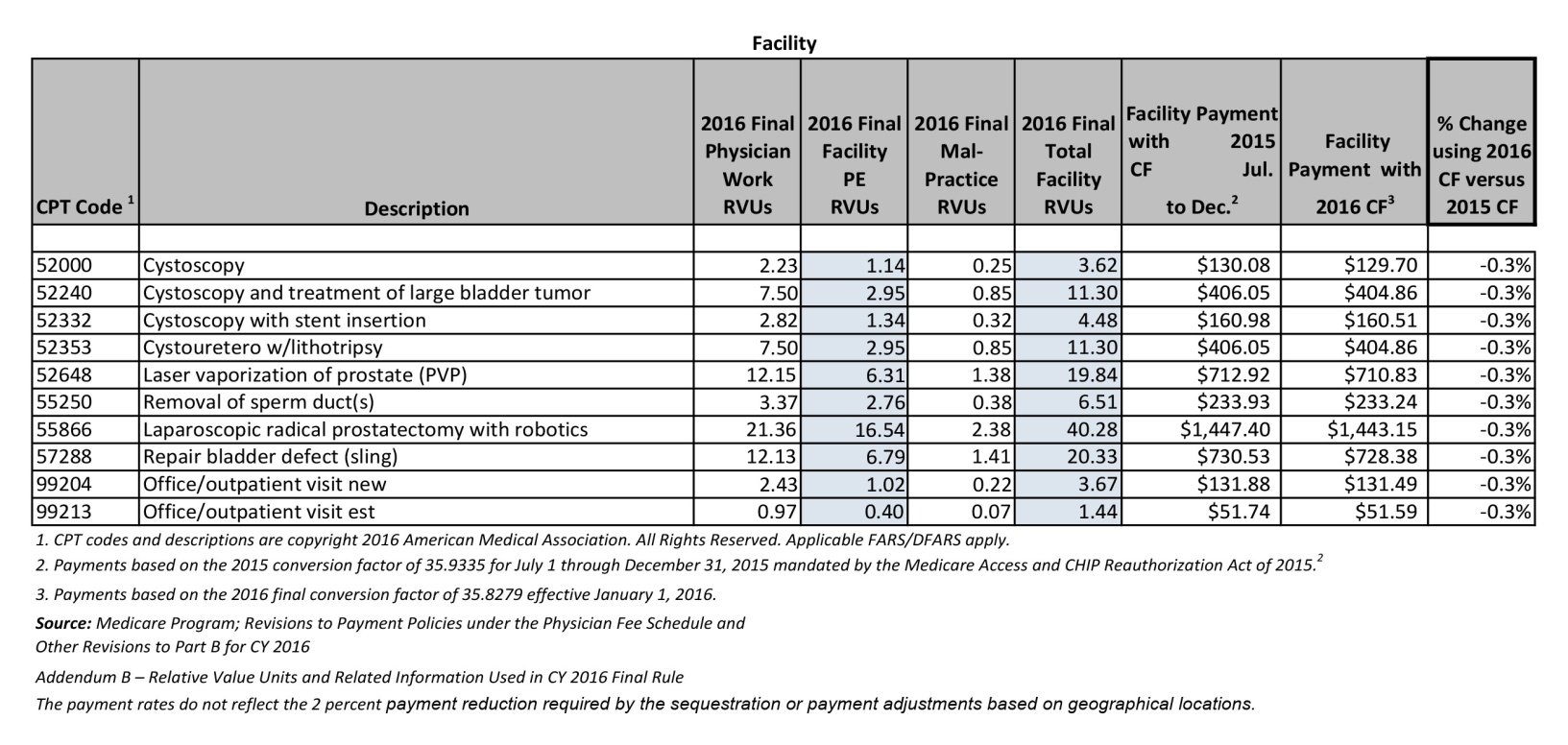
Many audits offered in the pharmacy market are really just pricing analyses conducted for the purpose of trying to secure the brokerage account for the employer. These audits examine sample bills closely to find errors in the amounts billed and the medical procedures coded. A coding accuracy audit can help improve the accuracy of your medical records. Purpose of audits name of medical practice promotes adherence to a auditing compliance program as a major element in the performance evaluation of all providersnpp documentation.
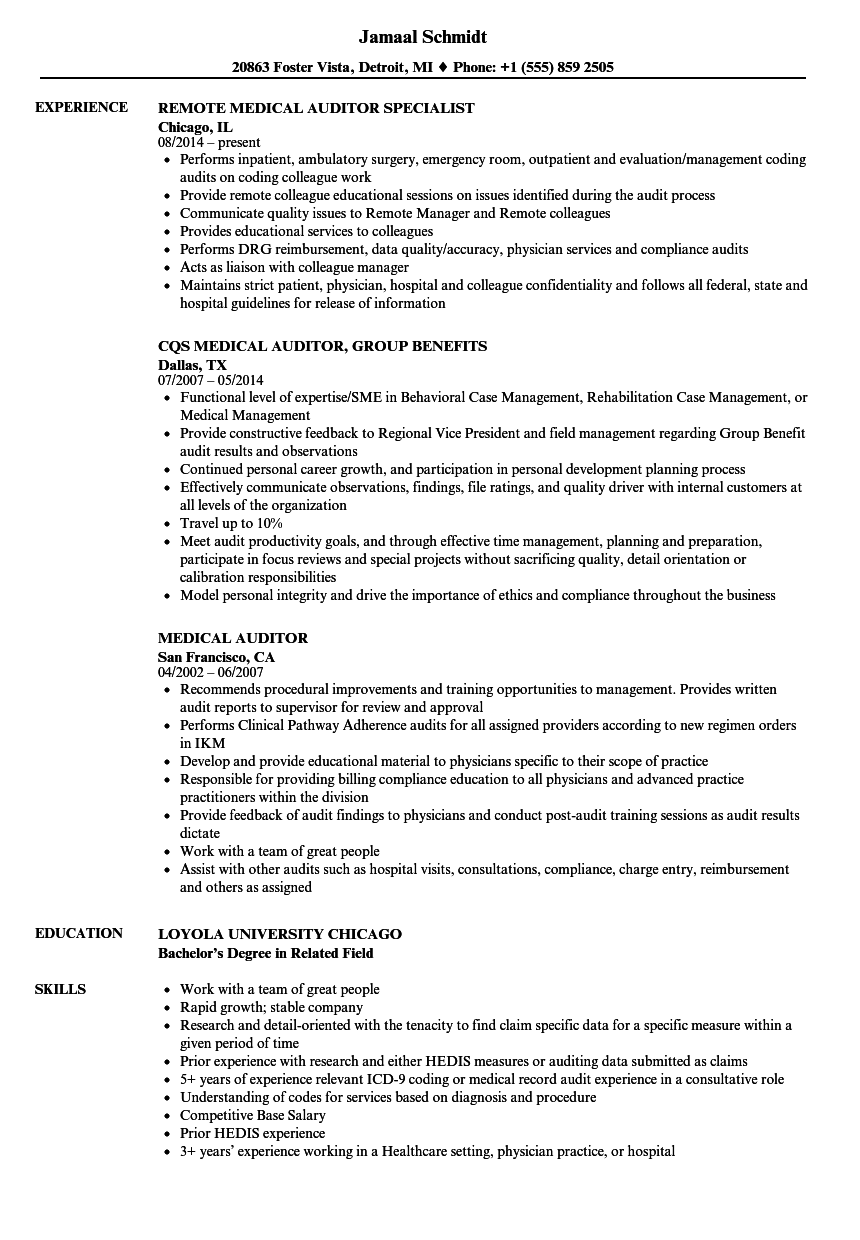
2 does the professional billing entity audit the medical record documentation to ensure that the appropriate em level has been billed. These audits may be performed either internally by the doctors office on its own bills or externally by an insurance company. We guarantee that if we dont find something wrong your audit is free. The practice employs a certified professional coder cpc to ensure accurate billing and coding.
A coding audit can bring your attention to what isnt in them. For physician practice audits 10 claims are usually enough. A statistical sample is also an option especially if your audit department has sophisticated software he says. A coding accuracy audit can help you better manage your staff.
Sample auditing compliance plan this is a sample only guidelines should be based on your medical practice mac guidelines and compliance committee a. Practice conducts regular audits to identify and resolve any billing errors. In either case include a mix of payers in the sample with more emphasis on medicare and medicaid as the federal government is the payer shining the strongest light on fraud.