Soap Note Template Social Work

Soap case notes template.
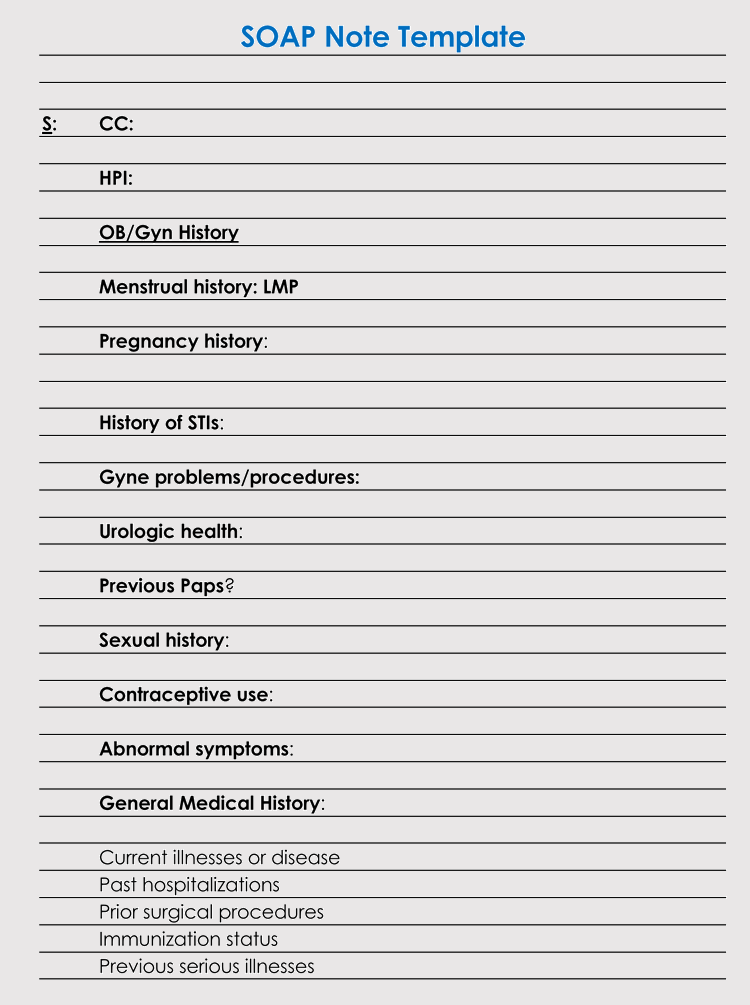
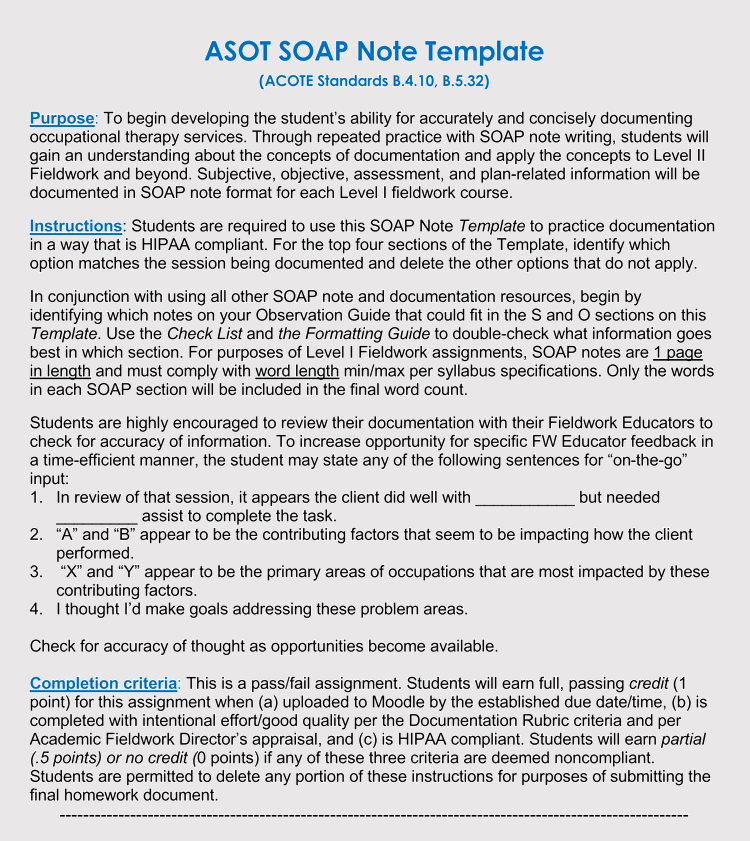
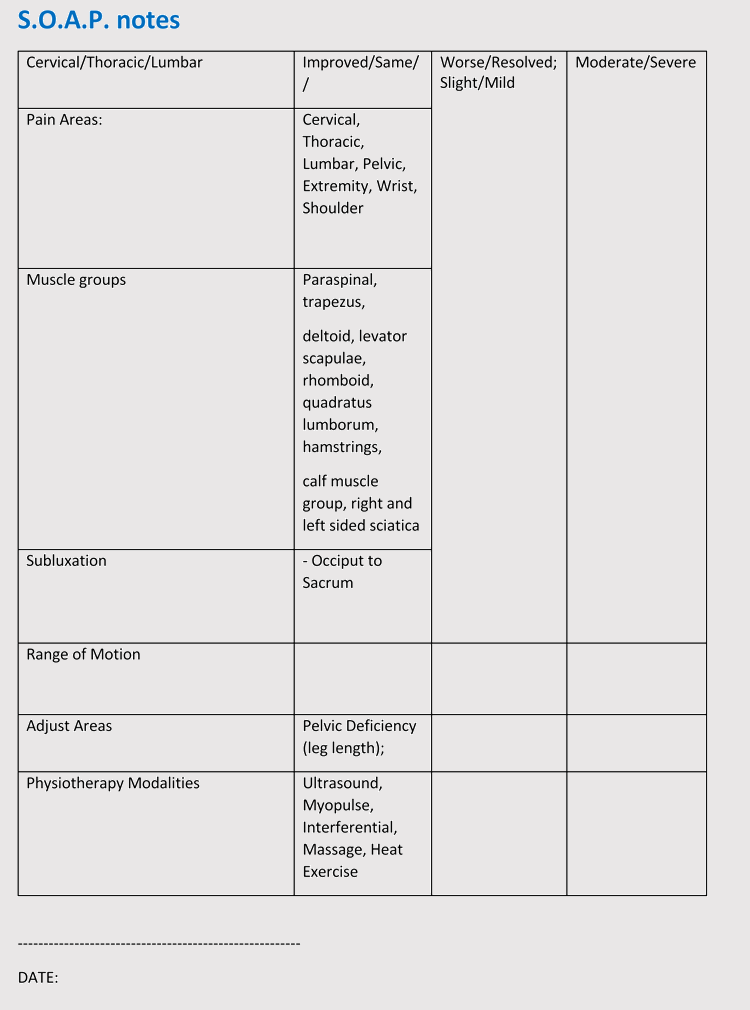
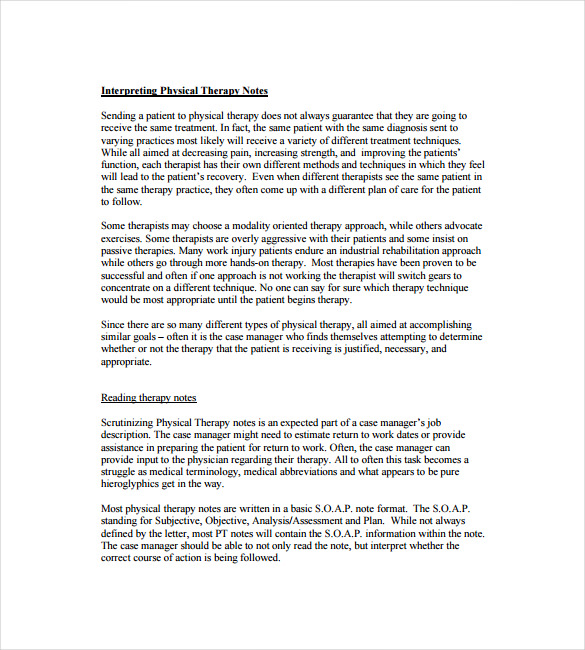
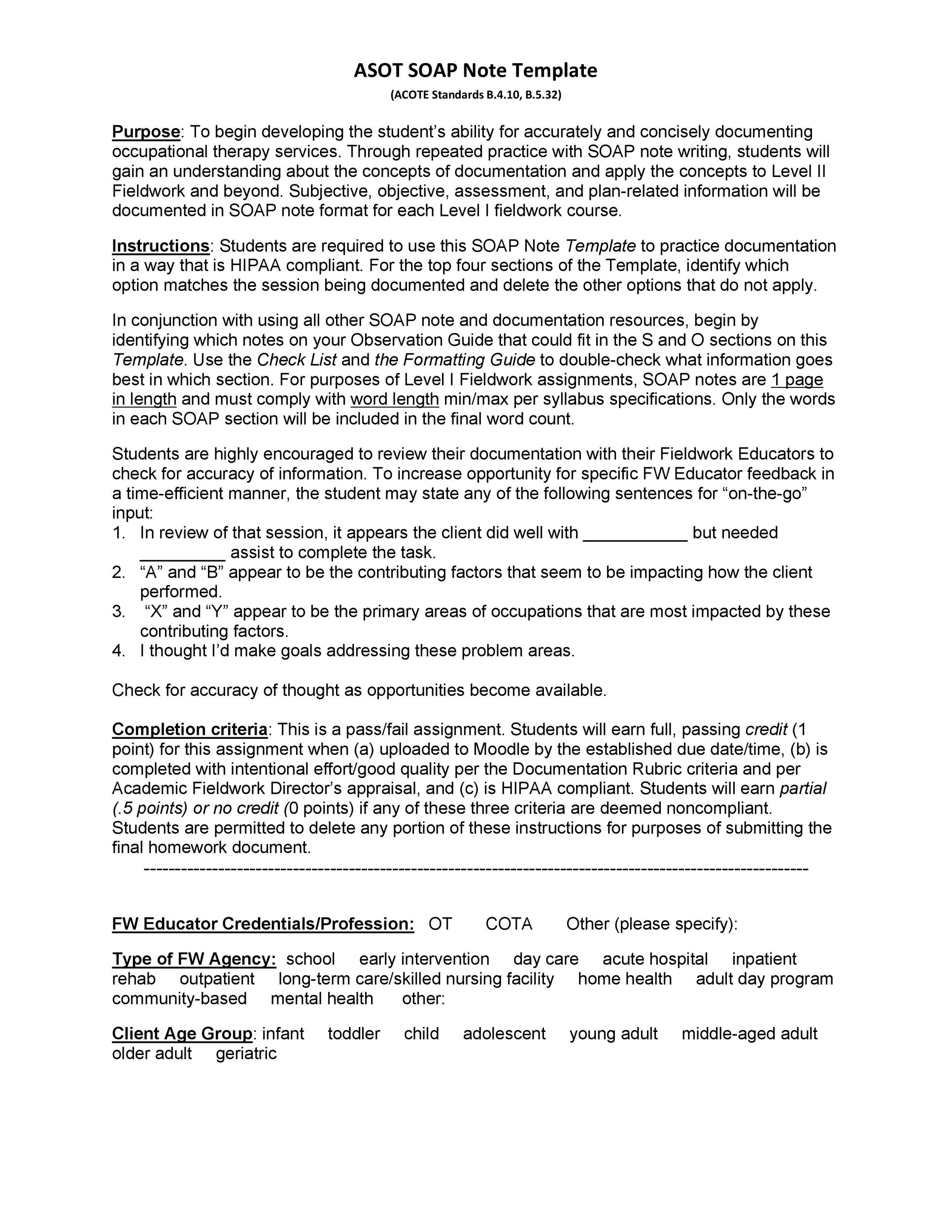
Soap note template social work. Learning to write case notes using the soap format. Soap notes physiotherapy template. Structured counseling notes whether soap or dap notes always end with the plan for the next session. More commonly mental health soap notes are required for insurance reimbursements in the case of a third party audit.
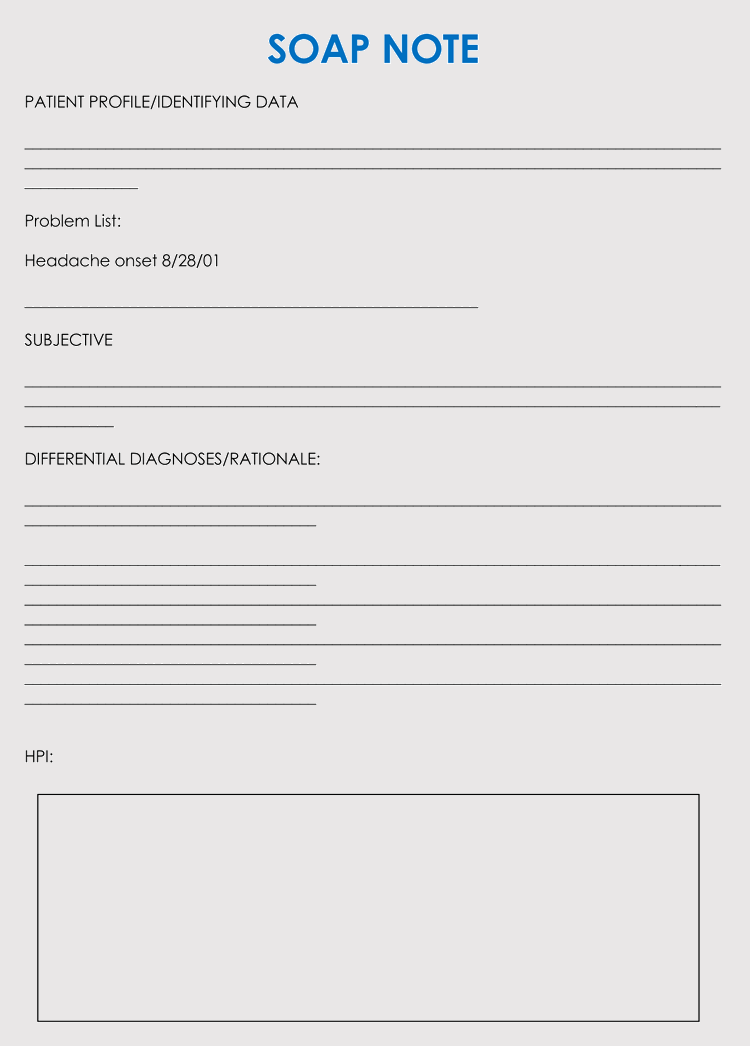
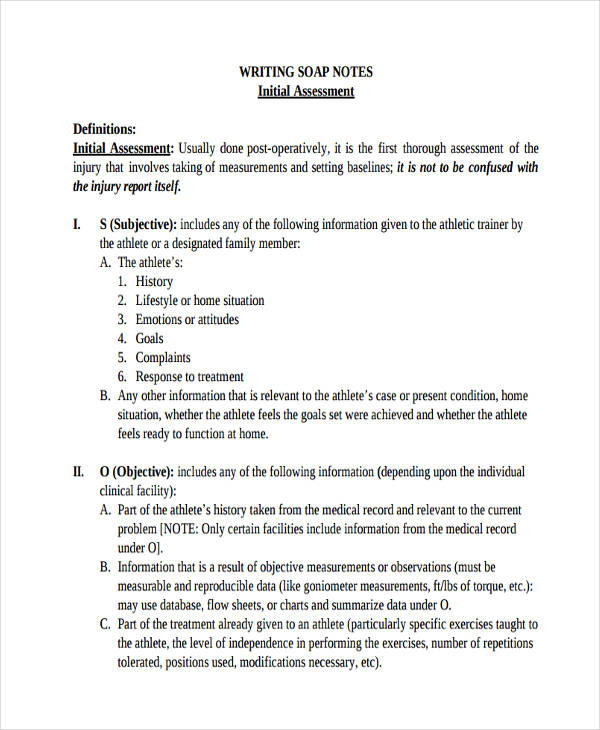
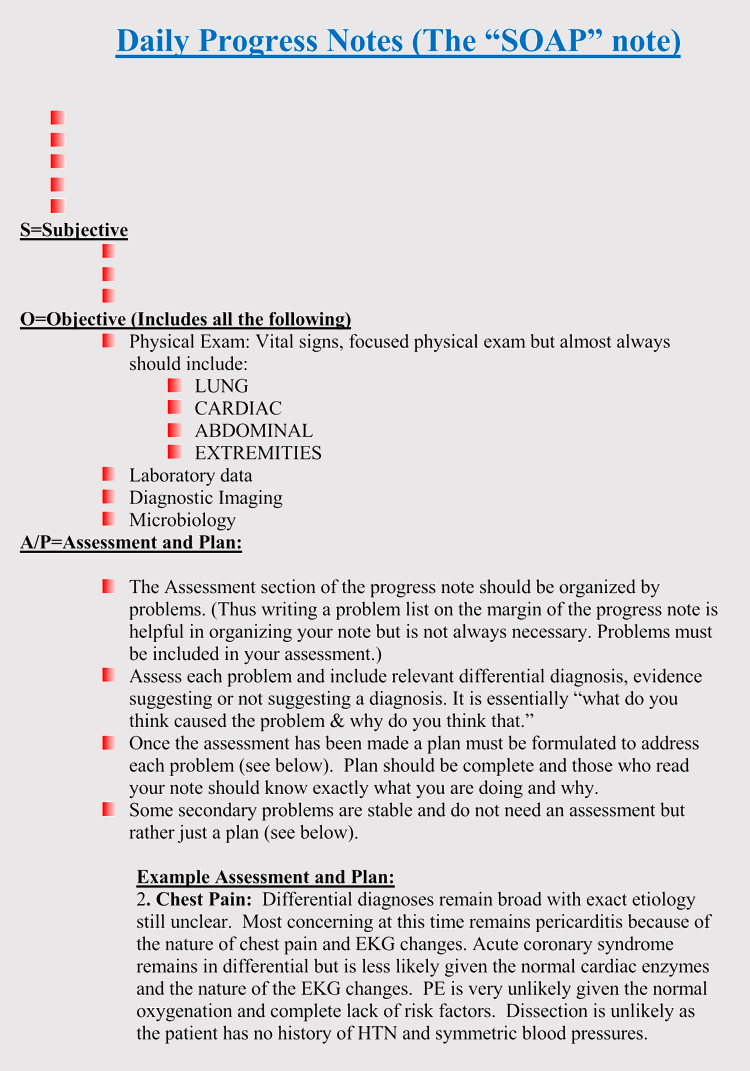
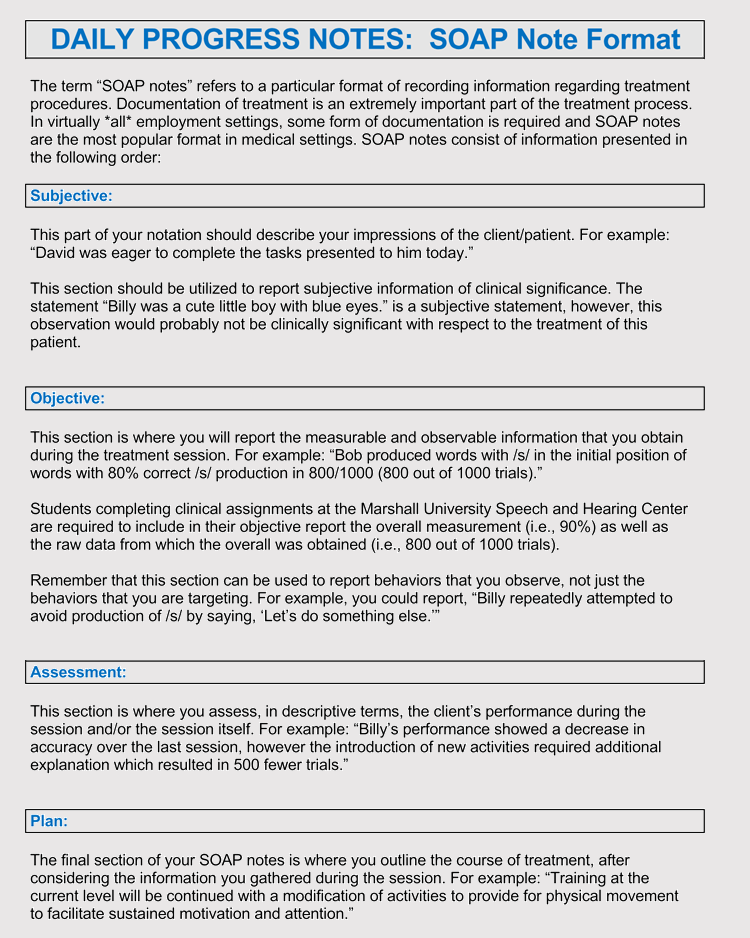
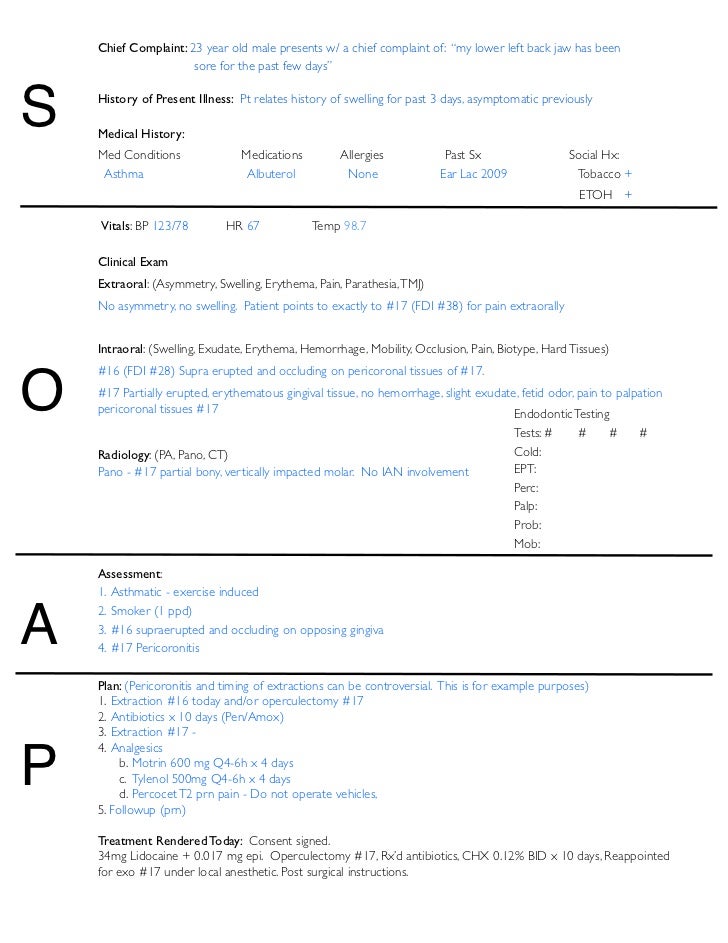
Note s subjective or summary statement by the client. The soap notes template is an easy and an effective method for quick and proper treatment for a patienta soap note is usually made up of four divisions the subjective part that has the details of the patient the objective part that has the details of the patient that are recorded while he is at the hospital the assessment part which is basically. Soap notes were first developed in 1964 as a means of providing accurate records of a patients history case details prognosis treatment and results. Also referred to as progress notes.
Usually this is a direct quote. Based on what was. Soap notes also create a paper trail of documentation that may be useful in the case of a malpractice suit. Posts related to soap notes template social work.
If adding your own explanatory information place within brackets to make it clear that it is not a direct quote. Sample soap note for social workers. Through the use of each of the four areas in this record keeping method a social worker documents initial problems steps taken to resolve the problem and the final results of these treatment steps. As you the therapist work through the note in a structured manner that process of recording facts will usually lead to what needs to happen next.
The therapist lists down his findings of the patient in the set format. Soap notes template pdf. Totally free soap notes templates. Whether you are a licensed clinical social worker or an msw social worker if you have a case load chances are you need to write case notes.
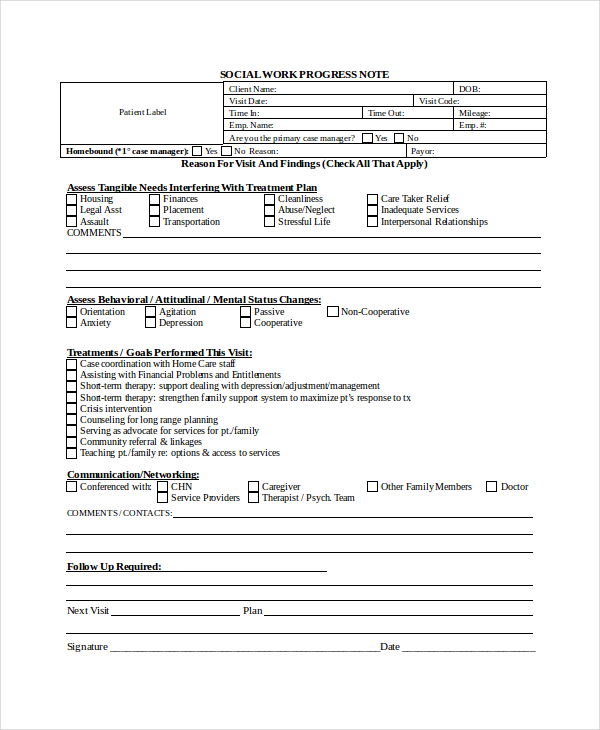
Switching to this note taking technique is better for both your patients and your practice. This would enable him to take corrective measures to improve the condition of the patient. It lists down the tangible needs his behavioral changes for assessment as well as the line of treatment. November 9 2018 by role.
This document is a sample template of a social work progress note. Soap notes template social work.